Our Network
Autism/ABA/BCBA Providers
Optum is recruiting Board Certified Behavior Analysts (BCBA) in solo private practice and qualified agencies that provide intensive ABA services in the treatment of ASD, for our Autism/ABA provider network.
Individually-Credentialed Clinicians
To apply as an individual, you must be a solo clinician or practicing within a group that does not currently have a group agreement with Optum.
Facility or Hospital-Based
To apply for Facility or Hospital-Based, your facility must offer MH or SUD Inpatient, Residential, Partial Hospitalization or Intensive Outpatient Levels of Care.
Group with Individually Credentialed Providers
To apply for group with individual credentialing, you must be part of a group that has a group agreement with Optum.
Group with Agency Credentialed Providers
To apply for Agency credentialing, your group must be designated as a Community Mental Health Center (CMHC), Federally Qualified Health Center (FQHC), Rural Health Center (RHC), Opioid Treatment Program (OTP), and/or other Federally or State licensed or certified entity (license or certification is at the organizational level).
Learn more about our Specialty Network Requests
Credentialing Plans
These plans provide an overview of Optum Behavioral Health policies for provider credentialing, recredentialing and ongoing monitoring. The process described in these plans will be initiated only after we make a preliminary determination that we want to pursue contracting or re-contracting with the applicant. Please review for more information.
Initial Credentialing Status
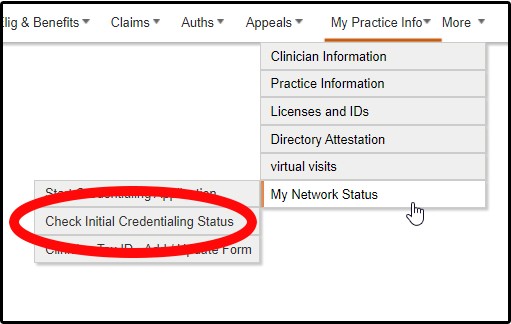
Individual providers – Using the Initial Credentialing Status Toolbar you can easily track the status of your online submission as it moves along the approval process. Log into the secure transactions area of Provider Express, hover over My Practice Info >> My Network Status >> click on Check Initial Credentialing Status.
Agency or Group Practice – contact Network Management at (877) 614-0484
Facility – contact Network Management at (877) 614-0484
Autism/ABA - contact Network Management at 877-614-0484
Medicare Plans and Intensive Outpatient Services
Beginning Jan. 1, 2024, any participating (contracted) Medicare-certified Opioid Treatment Program (OTP) may be credentialed to deliver Intensive Outpatient Services (IOP).to Medicare members in an OTP setting for the treatment of Opioid Use Disorder (OUD).As outlined in the Medicare Benefit Policy Manual Chapter 17 - Opioid Treatment Programs (OTPs) released by CMS, this new provision applies to facilities and agencies effective Jan. 1, 2024. The intent is to help increase access to behavioral health services for Medicare members.
Review the OTP-IOP Quick Reference Guide for the credentialing requirements for both network and out-of-network providers, treatment guidelines and billing guidance.
Review the Quick Reference Guide.
State-Specific Provider Information
Arizona Network Availability – 4/13/23
Optum Behavioral Health is limiting additions to our Arizona Medicaid network. Click here for more information.
We are only accepting new Medicaid network participation request forms for:
- Autism / Applied Behavior Analysis (ABA) / Board Certified Behavior Analyst (BCBA) and Autism Diagnostic Service providers in areas where we have a network need
- Providers joining an existing participating group(s)
Our commercial and Medicare Advantage networks remain open to all types of behavioral health providers.
State-Specific Provider Information information for UBH/Optum network providers to aid in working with members


