
July 2024 Issue
Nebraska: Are your claims being denied for one of these common reasons?
Every Provider Admittance Advice you receive from Optum Behavioral Health details the claim(s) that have completed the adjudication review process. It outlines the reimbursement(s) made to you and the amount the member is responsible for. It may also have a short code* to provide additional insight into the claim review, such as the payment amount or if the claim was denied and why.
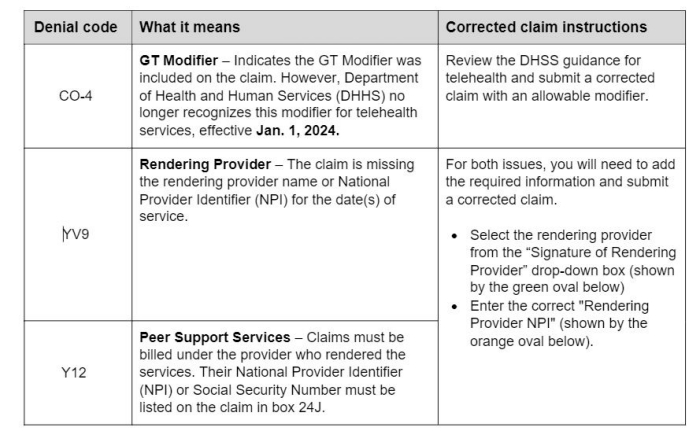
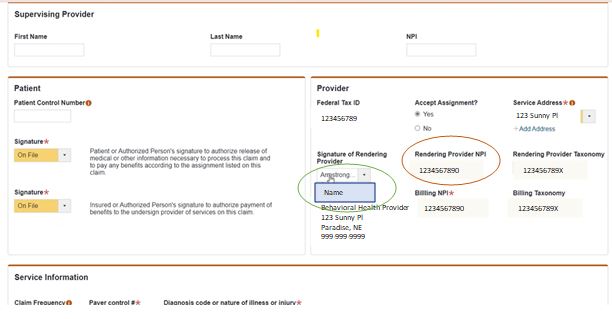
Claims are often denied due to missing or incorrect info. Take a look at some of the most common issues identified over the last several months. If appropriate, you can adjust the information and submit a corrected claim for another review.
Questions?
Contact your Provider Advocate at ohbs.centralregion@optum.com.